We can make a more accurate diagnosis by carrying out some skin scrapes on the affected areas. By using a scalpel and liquid paraffin we scrape the superficial layers off the skin. A skin scrape is painless. We then look at this debris under the microscope. In Demodectic mange we will see lots of cigar shaped, living mites.
Other pups from the same litter may also have developed the disease.
Not everything is understood about this demodeciosis. In fact, every year there is a worldwide conference held to discuss new theories and findings about this condition.
The current understanding is that the disease is as a result of a suppressed or underdeveloped immune system. In years gone-by we believed the mite to be the sole cause of the disease. Now we know that the mite is present in normal healthy skin albeit in much smaller numbers, and that there are other factors that upset the “normal” balance of healthy skin. This in turn makes conditions more suitable for the mite to survive and multiply.
The most common underlying problem is bacterial skin infection or pyoderma. Other less common conditions associated with the disease are immune suppression caused by cortisones, imbalances of hormones, or cancer. Occasionally there is an underlying allergy.
TREATMENT REGIME:
Long term antibiotics to treat pyoderma.
Shampoo … such as Pyohex.
Daily ivermectin by mouth to kill the mites. DO NOT GIVE TO COLLIE BREEDS.
Alternatively use oral Milbemycin or amitraz shampoos.
Return inspection after 3 weeks and repeat skin scrapes. Dead mites mean a positive scrape. We will need ongoing inspections.
Treatment should only be stopped after two negative skin scrapes 2 – 4 weeks apart.
DRUG TO AVOID:
CORTISONE. This tends to make things worse.
Photo from Penny Lane Collies
Young dogs generally do well and as their immune system develops they make a full recovery and don’t relapse. Some however can relapse after flea infestation, or at times of season, or develop an underlying Atopic (inhaled pollen) allergic dermatitis. The latter prove difficult to control as traditionally prednisolone (a cortisone) is used for control and as said before cortisone is a no-no. Anti-histamines in dogs are ineffectual.
In the cases of older dogs developing the disease that prove to be resistant to control, we have to look further (usually by blood tests) for another underlying cause. The most common underlying condition is a disease of the adrenal gland called hyperadrenocorticism or Cushings disease. The most difficult underlying condition to diagnose is an internal cancer that is not apparent by examination, blood tests, x-ray or ultrasound. The prognosis for all older patients is always much more guarded.


FELINE UROLOGY SYNDROME (FUS)
Also known as Feline Lower Urinary Tract Disease (FLUTD)
This is an inflammatory disease that affects the kidney, bladder and urethra of the cat.
The symptoms are those of cystitis (inflammation of the bladder). The cat is seen to be squatting more often, passing small amounts of urine that may be bloody, and is often urinating inappropriately.
Severe cases of FUS present as cats with an extremely sore abdomen. They may be crying in pain or are even collapsed. This happens in the male cat as a result of blockage of the urethra at the penis. This is a medical emergency.
FACTORS ASSOCIATED WITH FUS
There is continued debate to the cause of FUS however most vets point the finger at commercial pet foods especially dry food. The condition is rarely seen in cats fed on raw chicken wings and table scraps. It is my belief that there is a reaction in the cat’s kidney to unnatural cereal proteins, colourings or preservatives. Crystals are formed in the urine and are then passed down into the bladder where they produce cystitis and urethritis. Severe inflammation of the urethra together with crystals and inflammatory exudates causes a blockage in the male cat. The urethra of the female cat is shorter and wider and doesn’t block. Failure to pass urine leads to back pressure and kidney damage.

BLOCKAGE
NO BLOCKAGE
BACK PAIN, ATAXIA AND YELPING
Associated with periodontal disease in a Maltese Terrier
Zoey, a female desexed, 8 year old Maltese terrier was first presented to me in May 1997 with yelping and a mild ataxia of the hind limbs.
The owner explained that she had presented Zoey initially 11 months prior to another veterinary practice. At that time, and according to their records, Zoey’s symptoms were of lethargy and hind limb ataxia. She was usually a very active dog. The owner had reported that her back legs were tending to ‘skait apart and she found it difficult to get up on a smooth surface, but was better on carpet’. On examination she had a fever of 39.8 and had pain on palpation of her midback. Her mucous membranes were a ‘bit yellow. Blood was taken and she was found to be anaemic with a PCV of 25%. Furthermore there was a strong positive Coombs test. She was diagnosed as having Auto Immune Haemolytic Anaemia (AIHA). Treatment with prednisolone and Imuran was initiated. A heartworm serology test performed was negative.
One week later the records show she was improving. Her weight was 3.5kg. However the owner reported to the other vet that she tended to yelp in pain even when not being touched.
A vertebral lesion was considered as a possible diagnosis of this yelping. 10 days later it was considered that Zoey was well enough to undergo an anaesthetic for x rays and a myelogram of her spine. It was discovered that she had a type 2 disc protrusion at T11/T12 and a lesser expulsion at T9/T10. Surgical options were discussed. And there was a 10% possibility of a tumour being the cause of the symptoms. The owner was to consider this option over the next 2 weeks while Zoey was still recovering from AIHA.
2 weeks later Zoey was represented. She was more active and had gained weight. The owner reported ‘she rolls on [her] back when playing and rubs [her] spine along the ground with no obvious discomfort’. The vet also found that it was ‘hard to assess spinal pain today’. It was also recorded that ‘Zoey anticipates pain and constantly cries before she is touched.
2 weeks later the practice records indicate her PCV to be 42%. The treatment regime for AIHA was mapped out for the next 4 months.
4 months later (May 1997) I examined her. She now weighed 4.4kg. She was no longer on medication having been weaned off as directed. The symptoms of mild ataxia in the hind limbs and yelping for no apparent reason had returned. The yelping had no distinct pattern and was not linked to any particular action, such as eating or walking. It could happen at any time.
On examination she had a fever of 40.2, had a medial luxating patella (grade 1) of the left hind leg and had no apparent pain on palpation of her back. She had severe halitosis which was associated with extensive periodontal disease.
With her history of AIHA I checked her PCV in house. This was a ’normal’ 43% and her Total Protein was 65. Further blood tests were sent to the laboratory and and x rays of her spine were performed. I considered the changes in her vertebral spaces were ‘not active’ as there had been no deterioration of neurological symptoms since the 8th of August 1996. Furthermore after treatment for her anaemia began, she had not had ataxia or any other neurological deficits. The blood tests results were as follows: * indicates not in reference range
Full Blood Count:
Red Cells : Anisocytosis+, Poikilocytosis+
White cells : Leucocytosis+, Monocytosis++, Eosinophilia+, Left Shift+
Biochemistry:
I evaluated the significance of all the information from the clinical examination, the blood tests and the x rays and I felt that I should treat the obvious problem before looking for another diagnosis of Zoey’s condition. Periodontal disease was both obvious and I believed significant. I therefore discussed this with Zoey’s owner and also explained periodontal disease’s effects to the entire body. I recommended a thorough dental overhaul in order to treat the severe periodontal disease.
Under general anaesthetic I was able to conduct a full oral examination. There was extensive pyorrhea and deepened periodontal pockets in many places. Some teeth were loose in their sockets. “Unsavable” teeth, including the canines, were extracted. The surviving teeth were descaled and polished. Parenteral antibiotics (Penicillin and Amoxycillin) were administered and Zoey was prescribed Stomorgyl for 5 days. Furthermore a change of diet was recommended to daily raw chicken necks or wings, and cooked vegetable table scraps. Over the years it was clear to me that this daily diet was the best way of preventing periodontal disease. Zoey had periodontitis. Periodontitis is regarded as irreversible, unlike gingivitis. However with the correct management its progression can be slowed. Tooth brushing was considered as an adjunct especially for plaque control on the incisors. However Zoey was very mouth shy and could be vicious if she wanted! I recommended the owner to give up feeding all commercial foods. It was my opinion, with experience, that these mushy foodstuffs contribute to the problem of disease of the gums. Feeding dry, cereal based, kibble is not to any advantage in preventing plaque formation. After all have you ever brushed your teeth with a biscuit? A repeat inspection was planned in a week.
In that week Zoey had made an excellent recovery. The owner changed her diet which she took to despite her missing teeth (we had saved her opposing upper premolar 4s and lower premolar 3s). She was no longer ataxic and, more importantly, her yelping had stopped. She was again active and jumping as ‘if she was a puppy’.
18 months later Zoey again presented to me with yelping. She did not have a fever. There was pain found on palpation in the midback area. I was concerned about this because of the history of disc disease. I sedated her and performed x rays of the spine. There had been no deterioration from my x rays of 18 months prior. There was also no ataxia or other neurological deficiencies. I treated Zoey for a soft tissue injury. She was medicated with Zenecarp, rest and confinement. She made a full recovery.
In July 2001 Zoey represented. She was now 12 years old. The owner was concerned that she had been yelping again, and that she may be drinking more. The owner reported she was more picky with her food (although she had eaten that morning) and seemed to sleep more. She had developed cataracts. On examination she was even less vicious! She had a significant fever of 39.3. Lumps had been identified consisting of 2 warts and a small, unknown, subcutaneous mass. The latter was more of a concern as it had appeared suddenly. It was decided that I was to anaesthetize Zoey and remove the lumps, and more importantly, with her history of yelping, fever and periodontal disease, perform a full oral examination for the presence of periodontal disease.
This was done the following day. Her teeth and gums were generally good for her age and breed. However an incisor was found to have deep periodontal pocketing and upon removal, a root abscess was identified. Antibiotics were prescribed.
Stitches were removed 10 days later where the owner reported that Zoey was back to her ‘old self’. She was even trying to take on’ her 9 year old mate. She was no longer lethargic, was eating better, and her water intake had returned to normal. Histopathology revealed the subcutaneous lump to be an intermediate grade mast cell tumour. It had been completely removed with adequate margins.
2 years later in July 2003 Zoey started to have seizures. In one week she had had 4 fits that according to the owner’s description, resembled grand mal attacks. Under sedation blood tests (full blood count and biochemistry) were performed and found to be unremarkable. This pointed to an intracranial aetiology. Her mouth was examined and found to be free of periodontal disease. A referral to a specialist neurologist was recommended. However prior to the appointment Zoey had multiple fits in one night and presented to me in a severe comatose state. It was agreed that she be humanely put to sleep. My presumed diagnosis was of brain neoplasia.
Discussion:
1. Yelping, depression, ataxia and fever were related to periodontal disease. This was demonstrated twice in Zoey’s case. The second time only required one small incisor tooth root infection to trigger off the symptoms. In both cases Zoey made a full recovery after treatment of periodontal disease.
2. This dog also had similar yelping symptoms with back muscle pain. The distinguishing symptoms were demonstrable midback pain on palpation and NO FEVER. This was not related to periodontal disease.
3. Interestingly we saw the development of AIHA when periodontal disease was present. This suggests that periodontal disease should always be considered as a possible trigger to this auto immune state.
4. With the benefit of hindsight, I was able to prove that the disc lesions were from previous history and were not contributing to the clinical signs. If they had been active there would have been on going problems in the hind limbs, that, in turn, would not have resolved with my treatment regimes.
UROLITHIASIS (Bladder Stones)
Can Anyone Beat This?
Jupiter, a 10 year old desexed female poodle, was presented with a history of urolithiasis for 1 month. Jupiter weighed 21 kg.
Palpation revealed the presence of a mass in the bladder area. A presumptive diagnosis of urolithiasis was made. Jupiter was admitted for x rays under a general anaesthetic. This confirmed the presence of a large bladder stone. Cystomy followed and allowed the removal of a single very large, smooth bladder stone. Recovery was uneventful. Jupiter was put on a 14 day course of antibiotics (Amoxyclav, Apex) and has made a full recovery.
A sample was not sent to the laboratory for analyses but I would assume it to be a struvite urolith and its aetiology to be as a result of infection. The stone measured 100 X 50 X 50mm and weighed 150g. It was so big it was assuming the shape of the bladder! She was very relieved to have it removed. She now weighs 20.85 kg!


PERIODONTAL (GUM) DISEASE PREVENTION
Studies and observations in practice show that periodontal or gum disease exists in greater than 85% of our pet dogs and cats older than 2 years of age. Periodontal disease is the most common disease seen in general pet practice in Australia.
The pictures below indicate the stages of gum disease ranging from gingivitis (inflammation of the gums) to severe periodontitis (inflammation/infection of the tooth sockets). Pictures courtesy of Pfizer Pty Ltd.
A bad smell on the animal’s breath is often the first thing noticed by the pet owner. Other symptoms recorded are yelping when eating, swellings from root abscesses, excessive licking of lips, discharging sinuses in gums or below the eye (malar abscess) weight loss, inappetence and general lethargy and ill health.
A closer examination of the mouth especially the outside of the back and upper teeth (premolars and molars) may also reveal a thick covering of tartar (brown in colour) on the teeth, pus around teeth, generalised ulceration, gum recession, pain or even loose or missing teeth.
However the animal often shows no pain. They have no choice. Pus and poisons will circulate throughout the body leading to general ill health. Constant pain is debilitating. Periodontal disease is a slow and insidious disease that is most often hard to detect especially if there are no dramatic symptoms. It is commonly misdiagnosed as part of the ‘ageing process’.
The outcome of performing dental surgery reinforces the diagnosis. “Like a new puppy” and “Hasn’t behaved like this for years” are comments received after only 7 days.
FACTORS ASSOCIATED WITH GUM DISEASE
At the Bligh Park Veterinary Hospital we believe that correct diet is by far the best way to prevent the development of this often silent disease. Use of this diet from an early age and after dentistry is recommended.
Research has shown that too much mushy processed commercially prepared food will result in an increased incidence of periodontal disease. Similarly weaning young 3-4 week old kittens on to red mince will contribute dramatically to early symptoms of gum disease.
For more information on prevention see Good Diet is the Keystone to Good Health and “Periodontal Disease Prevention in Cats”.
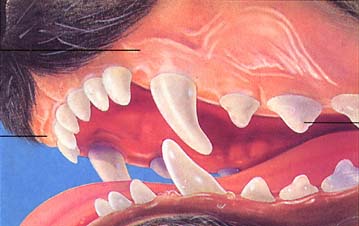
Noticeable Halitosis
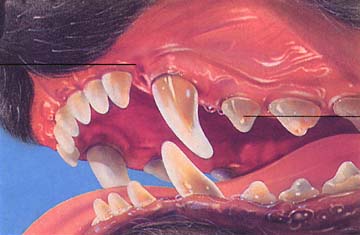
Obvious Halitosis

ANAL GLAND (SAC) DISEASE
Lady, a 4 year old beagle, was recently presented with a bloody discharging sore under her tail. She would not let her owner look at it. On examination Lady had a ruptured abscessed anal gland. The anal glands (or sacs to be more accurate) are the scent glands of the dog and cat (and skunk). They are situated on either side of the anus and would normally empty when the animal defecates. In Lady’s case the duct was blocked and the sac became infected and swollen. At this point the dog would ‘sledge’ their bottom on the ground in an attempt to relieve the swelling. This in turn causes the abscessed sac to rupture through the skin beside the anus.
Treatment involves an anaesthetic. This allows the vet to flush out the ducts and introduce antibiotics directly into the glands.
Lady went home with antibiotic tablets and instructions to bathe the wound with salty water. She subsequently made a full recovery.
Blocked anal sacs in smaller dogs are often a re-occurring problem. This presents as repeated ‘sledging’ (nothing to do with cricket!!) or even a skin infection
ARTHRITIS – A SORE PROBLEM!
Dogs and cats can suffer from arthritis and osteoarthritis, an ongoing inflammation of the joint or joints. We see more cases of arthritis in autumn and winter because of the cold nights. The symptoms of arthritis are:
Uncharacteristic ‘crankiness’ to humans and other dogs in the household especially if touched in the hind legs or pelvis.
There is treatment for arthritis that is both safe and effective. It is a degenerative disease that we cannot cure but can manage with medications either in tablet or injection form. Both forms of treatment are non steroidal anti inflammatory drugs (NSAIDS). The injectable medicine is a drug called Pentosan. The vet will favour this treatment as it has been shown to rejuvenate the worn surface of the joint as well as suppress pain. Four injections one week apart have a lasting effect for perhaps 4-5 months.
The other alternative treatment is a daily tablet. This does not affect the joint lining but removes pain and allows the animal to have pain free mobility. Ongoing daily administration is required although it is usually once daily. Gastric ulceration is not a problem. Relieving the pain of arthritis allows your dog to have a more active life.
Disease Digest
Disease Digest
Disease Digest
